IVF MORE®
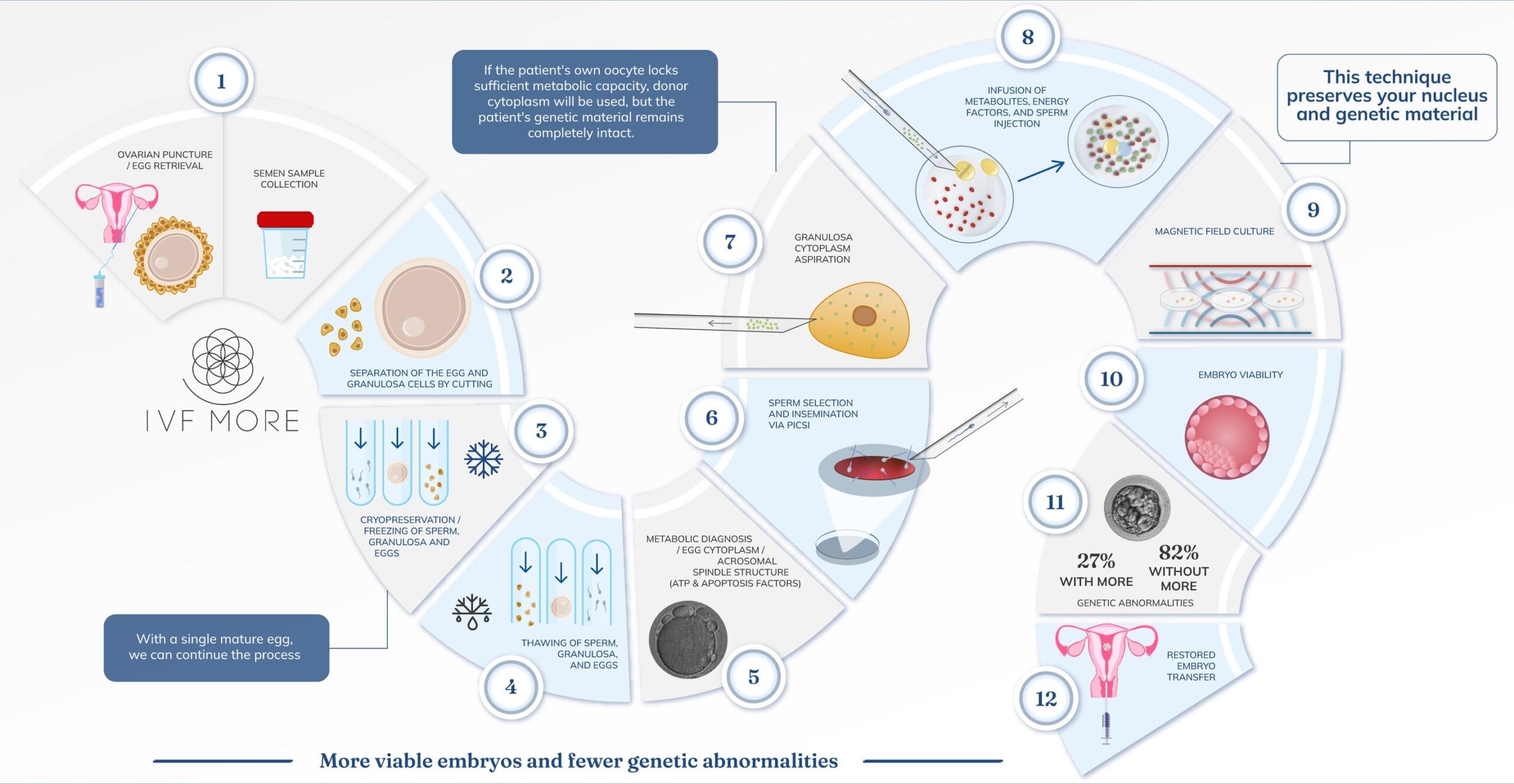
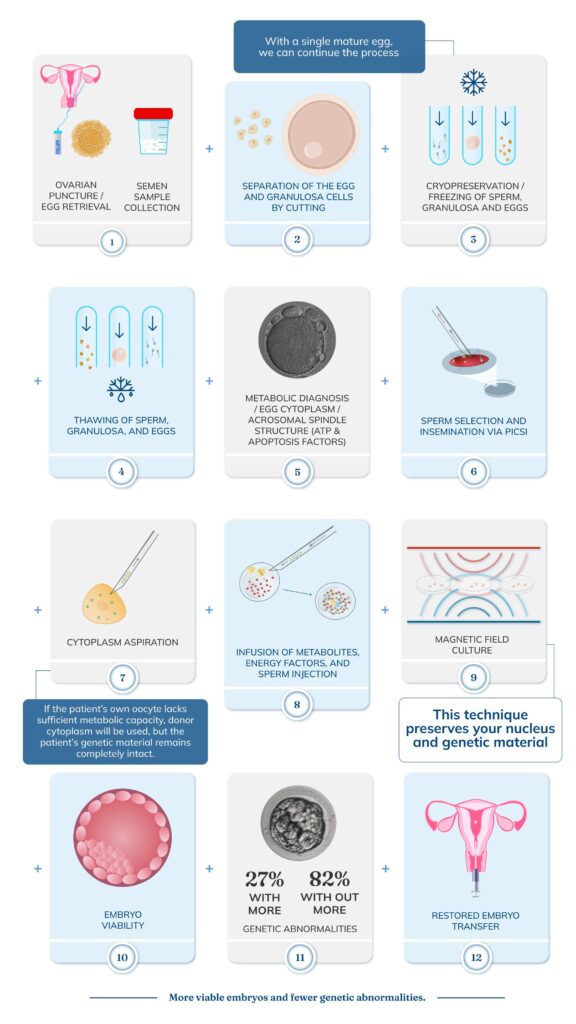
Is an innovative technique that restores low-quality eggs to increase the chances of pregnancy using the patient’s own eggs. Here’s a step-by-step explanation.
A clear step-by-step guide to understanding your journey with IVF MORE®
Click the arrows to see the entire step-by-step process.
Personalized Medical Consultation
It all starts with a consultation to evaluate your case and define the appropriate treatment.
Ovarian Stimulation and Egg Retrieval
The ovaries are stimulated to obtain eggs. With just one mature egg, we can proceed with the process. Once retrieved, the eggs are vitrified simultaneously with the sperm sample (if applicable).
Egg Metabolic Diagnosis
- Aging and Oxidative Stress: PubMed Link DOI: 10.1002/jcp.30468
- Metabolic Dysregulation in Oocytes of Patients with Low Ovarian Reserve: Zhu, Q., Li, Y., Ma, J., Ma, H., & Liang, X. (2023). Potential factors result in diminished ovarian reserve: a comprehensive review. Journal of Ovarian Research, 16(1). DOI
IVF MORE Treatment
Egg restoration is performed by infusing energy and mitochondrial factors to strengthen the deficiencies of the treated egg. In some cases, donor egg cytoplasm may be used without affecting the patient’s genetic material.
In Vitro Fertilization via ICSI
The best sperm are selected using advanced techniques, and fertilization is performed via Intracytoplasmic Sperm Injection (ICSI).
Embryo Culture in Magnetic Fields
Embryo Transfer
The endometrium is prepared, and one or more restored embryos are transferred. If there are any endometrial deficiencies, regenerative medicine treatments such as endometrial regeneration may be applied.
Complementary Treatments
IVF MORE® is not only a revolutionary advancement in egg restoration but also integrates complementary treatments to optimize egg quality, endometrial receptivity, and genetic embryo evaluation.

OVAGEN®: Improving Ovarian Function
For patients with low ovarian reserve or poor ovarian response, one of the main challenges for IVF MORE® is obtaining a sufficient number of functional eggs. OVAGEN® is a regenerative medicine treatment designed to optimize ovarian response by stimulating the body’s own repair mechanisms. This procedure is designed to:
Increase ovarian vascularization, improving oxygen and nutrient supply
Stimulate follicular development, enhancing egg production
Reactivate ovarian function in women with low reserve or poor response to previous treatments
The procedure involves the direct application of growth factors obtained from the patient’s own blood plasma (PRP), along with other bio-stimulants that promote ovarian regeneration.
How it complements IVF MORE®:
OVAGEN® expands the possibilities for patients who, due to their condition, would produce few or no oocytes. By improving both the quantity and quality of eggs, this treatment increases the number of oocytes available for restoration with IVF MORE®, enhancing success rates.
ENDOGEN®: Optimizing Endometrial Receptivity
The endometrium plays a critical role in embryo implantation. For a restored IVF MORE® embryo to implant successfully, the endometrium must be optimally thick, vascularized, and receptive.
ENDOGEN® is a regenerative medicine treatment that uses growth factors and, in some cases, mesenchymal stem cells to enhance endometrial quality, especially in patients with:
- Thin endometrium (<7 mm) or documented low receptivity
- Recurrent miscarriages due to implantation failures
- Conditions that alter the uterine environment, such as Asherman’s syndrome
How it works?
- Platelet-rich plasma (PRP) is collected from the patient
- PRP is enriched with endometrial growth factors and, if necessary, mesenchymal stem cells
- The solution is applied directly to the endometrium using a minimally invasive procedure before embryo transfer
How it complements IVF MORE®?
After restoring eggs and obtaining viable embryos with IVF MORE®, ENDOGEN® acts on the other critical component of pregnancy: the uterus. By improving endometrial conditions, implantation rates are significantly enhanced.
Endometriosis:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10342681/pdf/jcm-12-04186.pdf + https://pubmed.ncbi.nlm.nih.gov/23834505/ + https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5173290/pdf/nihms801246.pdf + https://pubmed.ncbi.nlm.nih.gov/31211846/
- Obesity attenuates the beneficial effect of an intrauterine infusion of autologous platelet-rich plasma during in vitro fertilization
- Personalized regenerative strategies, and molecular diagnosis for in vitro fertilization success a case report
Genetic Evaluation Without Biopsy:
Non-Invasive PGT-A
One of the main advances in fertility is the ability to analyze embryo genetic health without the need for a biopsy.
How it works?
Instead of extracting cells from the embryo, as in conventional biopsy, we use an advanced technique that analyzes the DNA released by the embryo into the culture medium.
Benefits of Non-Invasive PGT-A:
- Less stress on the embryo → No perforation of the embryo’s outer layer
- High accuracy in detecting chromosomal anomalies → Down syndrome, Turner syndrome, Klinefelter syndrome, and others
- Fast and reliable results → Without compromising the embryo’s viability
How it complements IVF MORE®:
MORE® reduces genetic abnormalities in embryos. However, for added security, we offer Non-Invasive PGT-A as an additional step in embryo evaluation.
Limitations:
Embryos may not release enough genetic material into the medium, which would require a biopsy to analyze their chromosomal load for traditional PGT-A diagnosis. For IVF MORE®, it is recommended not to biopsy the embryo due to prior manipulation during the egg restoration process.
Live Births Per intended Egg Retrieval SART : https://sartcorsonline.com/CSR/PublicSnapshotReport?/ClinicPKID=0&reportingYear=2022
Compatibility with Previously Frozen Eggs
If you previously froze eggs with the hope of using them in the future, IVF MORE® can help optimize their chances of success.
How it works:
- The procedure is carried out in our Ingenes laboratories. Once we have your eggs, either retrieved in Mexico City or transferred to our branch, we start the treatment.
- We perform a metabolic diagnosis to assess their quality.
- We apply IVF MORE® treatment to restore the eggs before fertilizing them.
When is it recommended to restore frozen eggs?
- If you froze eggs after the age of 35
- If your eggs show signs of low quality when thawed
- If you’ve had previous failed fertilization attempts with your frozen eggs
Are your eggs in another clinic or country?
No problem. At Ingenes, we work with companies specializing in biological material transportation, and we can coordinate the transfer of your eggs to Mexico, ensuring they arrive in optimal condition for restoration.
*Consult our egg transportation protocol from other international clinics.
A Personalized Treatment for Every Patient
Whether you need to optimize the quality of your eggs with OVAGEN®, improve endometrial receptivity with ENDOGEN®, or undergo non-invasive genetic analysis with PGT-A, each of these treatments complements the IVF MORE® methodology to give you the best chance at a healthy pregnancy.
Take the next step toward growing your family
We are here to support you every step of the way.
